 The question for today is whether academic medicine is at risk for extinction. To answer that question, let's take a deeper dive and look at how the average medical school funds itself.
The question for today is whether academic medicine is at risk for extinction. To answer that question, let's take a deeper dive and look at how the average medical school funds itself.
The data from the AAMC shows that only about 4% of the medical school budget is covered by tuition -- this may be surprising to many of you who are still paying off your student loans. The majority of the funding for a medical school is from clinical revenue, be it hospital contracts or faculty practice collections.
The real take-home message is that it's the clinical practice that cross-subsidizes the research and education mission in academic medicine. So, when the clinical mission catches a cold, the rest of the academic medical center gets pneumonia. The big problem is we're now in perennial flu season. And why is that? Well, let's look at how much we spend as a nation on healthcare.
By 2018 or 2019, about 20 cents of every dollar in the U.S. economy is going to be spent on healthcare. To put this in real-world terms, if you drink Starbucks coffee, you already shell out more for the cost of employee healthcare in each cup of coffee than you do for the cost of the coffee to brew it. If you drive a General Motors car, you pay more for the cost of employee healthcare than for the cost of the steel to make it.
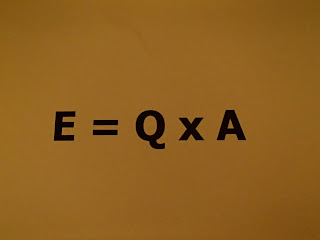
The American people, and employers who shoulder the majority of healthcare costs, are saying, "Enough is enough; we want more value for our money." And that is the shifting healthcare landscape we are all experiencing -- whether you're in academic medicine or not. It is a shift from fee-for-service to more emphasis on value. And the whole concept is about value. That is, improving outcomes while holding costs steady, or even reducing them.
So what does this mean for the average physician? First off, it means that we are going to get paid less for many things at baseline, and will only see a raise if we can prove outcomes are better. So, we're going to be measured in ways that we never dreamed of before, and certainly in ways that we haven't been exposed to in medical school and residency.
We're going to get scorecards from our hospitals, or other partners, about how much our average hospital admission costs, what our average length of stay is, how much we consume in supplies, and how often our patients are readmitted.
And we're going to be judged more on the total continuum of care, rather than quality in the acute hospitalization. It isn't just enough to get our patients safely out of the hospital -- they or their employers will judge us by how soon these patients get back to work and resume a normal quality of life.
Is academic medicine at risk for extinction?
Well, I think the answer to that question is largely in our hands.We're going to have to change our behaviors, pay attention to what the American people expect of us, and be willing to change.
(This piece originally appeared in Opinion Makers, a new MedPage Today video exclusive weekly series, presenting leaders from all areas of medicine offering their views on current topics in clinical care, research, and policy.
In a video (https://www.medpagetoday.com/publichealthpolicy/healthpolicy/53928) , Edmund Funai, MD, chief operating officer of USF Health at the University of South Florida in Tampa, discusses the future of academic medicine.

Comments
Post a Comment